As an embryologist, one of the most common questions I receive is about IVF embryo grading. Breaking down an embryo report can feel overwhelming, and searching the internet often leads to even more confusion. My goal is to explain embryo grading in a way that makes sense, minding that not all labs follow the same grading system. If you're ever unsure about what something means, ask your fertility clinic. And if they aren’t willing to answer your questions, that’s a major red flag. You’re investing significant time, money, and emotional energy into this process, and you deserve to understand your care. Now let's get into it!
How are IVF embryos graded?
Most IVF labs grade embryos following the guidelines established by the Society for Assisted Reproductive Technology (SART). While clinics aren’t required to adhere to SART’s system, it was developed to bring consistency to embryo grading. SART’s system assesses embryos on days 5, 6, and 7 based on three key components:
-
Expansion (how far along the embryo is in development)
-
Inner Cell Mass (ICM) (which will become the baby)
-
Trophectoderm (which will become the placenta)
This results in grades like 3AB, 4BB, or 2BC. Let’s break each of these down further.
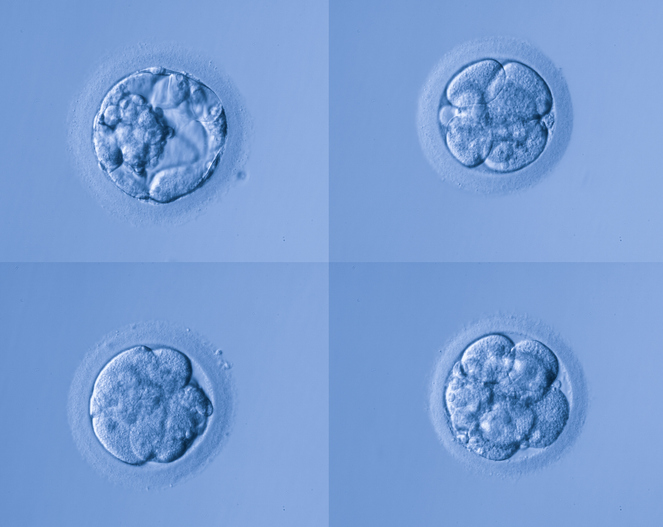
Expansion: Measuring embryo maturity
The number in an embryo’s grade represents its stage of expansion, ranging from 1 to 6:
-
1-2: Very early development; often not ready for freezing, transfer, or biopsy.
-
3-4: Common stages for freezing or transfer; indicates a good level of maturity.
-
5: The embryo is hatching out of its shell (zona pellucida). Some labs artificially assist this process with a laser on day 3, leading to earlier hatching.
-
6: The embryo is fully hatched. These embryos may have slightly higher implantation rates but are also more delicate and at greater risk of cryo damage.
While expansion grading indicates maturity, it does not necessarily reflect the quality or viability of the embryo. Some embryos may be slow to expand but still have excellent inner cell mass and trophectoderm quality, meaning they could still lead to a healthy pregnancy. Others may expand quickly but have poor cellular development, reducing their chances of implantation.
Inner Cell Mass (ICM): The future baby
The first letter in the grading system represents the inner cell mass, which eventually develops into the fetus. ICM quality is graded from A to D:
-
A: Well-organized, compact, with little cell death (ideal for implantation and development).
-
B: Less compact, but still viable.
-
C: Poorly defined or very small ICM. Some clinics may not freeze embryos graded as C.
-
D: Very poor quality, often not viable.
The inner cell mass is crucial because it will ultimately form the fetus. A strong, well-defined ICM increases the likelihood of a successful implantation and pregnancy. However, lower-graded ICMs still have the potential to develop into healthy babies, depending on other factors such as genetic normality and uterine environment.

Trophectoderm: The future placenta
The second letter in the grading system refers to the trophectoderm, which will become the placenta. Like ICM, it is graded from A to D:
-
A: Many healthy cells, minimal cell death, few gaps.
-
B: Fewer cells but still viable.
-
C: Sparse cell count with notable gaps or cell death, making biopsy difficult.
-
D: Poor quality, unlikely to support implantation.
Trophectoderm grading is particularly important for patients undergoing PGT (preimplantation genetic testing) because a healthy trophectoderm is necessary to retrieve enough cells for analysis while keeping the embryo intact. A strong trophectoderm not only supports implantation but also ensures the embryo has a better foundation for early placental development.
Best embryo grade
SART categorizes embryos based on ICM and trophectoderm grades:
-
Good quality: AA, AB
-
Fair quality: BA, BB
-
Poor quality: Any grade with a C (e.g., BC, CB, CC)
Expansion grading is not factored into these quality assessments, as it reflects maturity rather than viability. A highly expanded embryo with poor-quality ICM and trophectoderm may not implant, while a less expanded embryo with excellent cellular composition may still be viable.
Embryo grading: Good, fair, poor
SART provides a structured grading system to classify embryos into good, fair, or poor quality:
Good quality embryos:
-
Definition: Embryos that are free of or have only minor imperfections.
-
Characteristics:
-
Inner Cell Mass (ICM): Well-defined, compact, with minimal cell death.
-
Trophectoderm: Uniform, with many healthy cells and few gaps.
-
Fair quality embryos:
-
Definition: Embryos that are not top-tier but still viable.
-
Characteristics:
-
Inner Cell Mass (ICM): Moderately compact with some cell death.
-
Trophectoderm: Moderate cell count with some irregularities.
-
Poor quality embryos:
-
Definition: Embryos with significant imperfections that may reduce implantation potential.
-
Characteristics:
-
Inner Cell Mass (ICM): Sparse or poorly defined, sometimes absent.
-
Trophectoderm: Few cells, irregularly shaped, with notable gaps.
-
It's important to note that while these grades provide valuable information about embryo morphology, they are not definitive predictors of implantation success. Embryos with lower grades can still result in successful pregnancies, while higher-graded embryos do not guarantee implantation. This is why embryo grading should be considered alongside other factors, such as genetic testing results and uterine receptivity, when making decisions during the IVF process.
Additional considerations about embryo grading
-
Hatching embryos can look like they are splitting, but they aren’t. While identical twins result from embryo splitting, we cannot predict or influence this by looking at an embryo. Some hatching embryos may appear to be splitting, but this is a normal part of the development process.
-
Embryo grading does not determine gender. The only way to know an embryo’s sex is through PGT-A testing. Some patients assume that higher-graded embryos correlate with certain sexes, but grading is purely structural and has no connection to gender.
-
Embryo grading is just one piece of the puzzle. A poorly graded embryo can still lead to a successful pregnancy and a healthy baby! There are countless stories of “low-quality” embryos resulting in beautiful, healthy children. Conversely, some perfect-looking embryos fail to implant, reminding us that grading is just one factor in a complex process.
What does embryo grading mean?
Embryo grading is a valuable tool, but it’s not a crystal ball. While higher-graded embryos may have better implantation potential, lower-graded embryos can and do result in healthy babies. Always discuss your embryo report with your clinic to fully understand what it means for your unique journey. If you receive a report with lower-graded embryos, don’t lose hope — many people go on to have successful pregnancies despite less-than-perfect embryo grades.
Ultimately, embryo grading is a helpful but imperfect method of assessing potential. By understanding the different grading components, you can feel more empowered in your fertility journey and make informed decisions with your healthcare team. Best of luck!
Alease Daniel is an embryologist and experienced IVF laboratory technician based in Raleigh, North Carolina. In her free time, she enjoys baking and cooking with her husband and playing with her two pups! You can follow Alease on Instagram at @alease_the_embryologist or TikTok at @aleasetheembryologist.














.png)


